Drug coated balloon plays a very important role in the management of in-stent restenosis and native coronary artery disease, however its role in the treatment of complex coronary artery disease is an interesting and emerging concept. DCB are available for use in Europe and Asia, but not yet in the USA.
Drug eluting stents (DES) are the mainstay of treatment in a majority of patients with significant stenoses of the coronary arteries. However, the use of DES is associated with various acute and longterm complications such as stent thrombosis, in-stent restenosis (ISR), neoatherosclerosis, and abnormal vasomotion. Moreover, the implantation of DES mandates the patient to take dual antiplatelet drugs for a certain duration which is not always feasible in all patients and associated with an inherently increased risk in clinically relevant bleedings. Target lesion failure of DES ranges between 0.8-1% yearly in simple lesion subsets itself, with higher rates in the more complex lesion setting. The long-term results of DES are not optimal in complex coronary artery disease subsets such as chronic total occlusion (CTO), complex bifurcation lesions, long lesions, heavily calcific lesions, small vessel coronary artery disease and also, there are no enough studies available assessing the long-term outcomes of DES in this group. Drug coated balloons were initially developed to address the issue of ISR. Later the usage of DCB in treatment of native vessel coronary artery disease increased as it showed favourable long-term outcomes. The use of DCB in complex anatomy is a boon for the patients as it decreases the duration of DAPT needed and also works on the principle of the “leave nothing behind” strategy: in fact, no metallic cage is left behind in the arteries which in turn facilitates the vessel remodelling and also avoids the stent related complications. The current status of DCB use in complex coronary artery disease is reviewed in this article.
Drug coated balloon works on the principle of transferring an antiproliferative drug to the vessel wall upon inflation of the balloon. Paclitaxel is the drug used in the earlier generations of DCBs with a recent introduction of sirolimus.
Adequate lesion preparation is a prerequisite of any percutaneous coronary intervention (PCI) be it stent implantation or DCB application. The lesion is usually predilated with a semi-compliant or non-compliant balloon sized according to the distal vessel reference size in the ratio of 0.8:1 or 1:1. In case of non-yielding lesions further preparation with normal balloons, cutting or scoring balloons may be required. In heavily calcific lesions the use of rotational or orbital atherectomy, or lithotripsy may be required. The aim of lesion preparation is to achieve less than 30% of residual stenosis with TIMI III flow and no flow limiting dissection prior to the application of DCB.
There are various studies which have shown the efficacy of DCB in small vessel CAD. BELLO, BASKET-SMALL 2, RESTORE SVD, and PICCOLETO II are the most important among them. BELLO study compared the angiographic outcomes of 182 patients with small vessel coronary artery disease (SVD) defined as RVD < 2.8 mm, randomized to paclitaxel eluting stent (Taxus, Boston Scientific) vs Paclitaxel coated balloon (In.Pact Falcon, Invatec). The study showed superior angiographic results in paclitaxel coated balloon arm and also lower major adverse cardiovascular events (MACE) at 3 years. A large study, BASKET-SMALL 2, was performed on 758 patients, in which 382 patients were treated with paclitaxelcoated balloon (SeQuent Please, B.Braun), and 376 patients were treated with either the paclitaxel-eluting Taxus Element stent or the Everolimus-eluting Stent (Xience, Abbott Vascular). The rate of MACE after 12 and 36 months were similar between both groups (DCB versus DES: cardiac death 3.1% versus 1.3%, p=0.11; non-fatal MI 1.6% versus 3.5%, p=0.11; and target vessel revascularisation 3.4% versus 4.5%, p=0.448). In RESTORE SVD trial, 230 patients with RVD between 2.25 mm and 2.75 mm were randomized to RESOLUTE INTEGRITY (Zotarolimus eluting stent) vs RESOLUTE (paclitaxel DCB), at the end of 9 months DCB arm was shown to be non-inferior to the DES arm in terms of Target Lesion Revascularization (TLR), myocardial infarction, cardiac death and a composite endpoint. PICCOLETO II randomized 232 patients with SVD to everolimus eluting stent vs paclitaxel DCB (Elutax SV, AR Baltic). After a median follow up of 189 days, the in-lesion late luminal loss (LLL) was significantly lower in the DCB group. At 12 months follow up there was no significant differences found in MACE in both groups.
Bifurcation lesions are encountered in approximately 15-20% of the PCIs. A Bifurcation lesion is defined as a coronary artery lesion located at or adjacent to a significant side branch which the operator does not want to lose during the PCI. Treating the bifurcation lesions with stents poses many technical challenges and also carries high risk of stent-related complications due to high metallic load, malapposition, and neo-carina related altered hemodynamics. The Usage of DCB in bifurcation lesions avoids all the above-mentioned problems associated with the DES. In bifurcation lesions, DCB could be applied to both the main vessel and side branch as DCB only treatment or to the sidebranch alone in case of provisional stenting. Unfortunately, the data available is scarce and the robustness weak. Schulz et al. studied 39 bifurcation lesions with side branch diameter > 2.0 mm treated exclusively with DCB, angiographic follow up was done in 30 out of 39 bifurcation interventions at 4 months and it showed restenosis in 3 (10%), TLR was required in 3 patients corresponding to a MACE of 7.7%. In PEPCAD-BIF trial 64 patients with bifurcation lesions not involving the proximal main branch were randomized to DCB vs Plain Old Balloon Angioplasty (POBA) alone after successful predilation. At the end of 9 months angiogram showed LLL was 0.13 mm in the DCB vs 0.51 mm in the POBA group (p = 0.013). The Restenosis rate was 6% in DCB group vs 26 % in the POBA group. TLR was required in one patient among the DCB group vs three patients among the POBA group.
Chronic total occlusion lesions are seen in around 20% of the patients with CAD. Revascularisation of CTO with DES poses a challenge because there is higher incidence of stent thrombosis and ISR following DES implantation in this setting. Moreover, the distal vessel beyond the CTO grows during the first weeks following the establishment of antegrade flow and potentially leads to late stent malapposition and related complications. There is very scarce literature available regarding the use of DCB in CTO PCI. There are no randomized controlled trials available comparing the DES vs DCB in CTO PCI, only a few observational studies are available.
Philine J Köln et al. studied 34 patients with CTO treated with DCB, the recanalization was considered satisfactory in 79.4% (n=27) and not satisfactory in 20.6 % (n=7) patients. Restenosis occurred in 11.8% (n=4) and re-occlusion in 5.9% (n=2). Out of the 27 patients with a satisfactory initial result, 3.7% (n=1) had re-occlusion and 3.7% (n=1) had restenosis. In the subgroup without satisfactory result (n=7), restenosis occurred in 3 patients (42.9%) and re-occlusion in 1 patient (14.3%). A luminal increase was found in 67.6% (n=23) and mean late luminal gain was 0.11±0.49mm. Angina class improved significantly (p<0.001). There was no death or myocardial infarction.
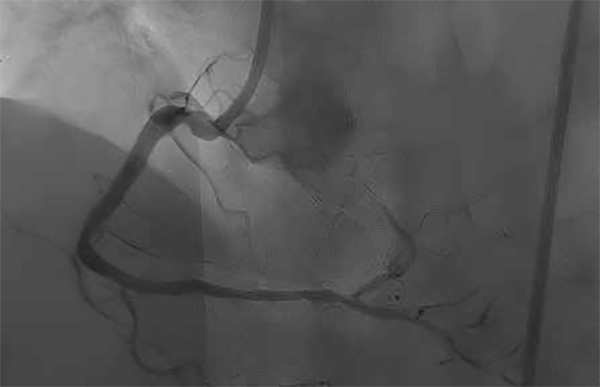
Eun Jung et al studied 84 patients with de novo coronary CTO lesions (93 vessels). Patients who had Thrombolysis In Myocardial Infarction (TIMI) flow grade 3 and <50% of residual stenosis following pre-dilatation with balloon angioplasty, and successfully treated with DCB without requiring stent implantation were included in the study. Patients had a median follow-up of 720 days (IQR, 406–1,268 days) after the index procedure. Angiographic follow-up was done in 72% of the patients. MACE occurred in 8.3% and 16.7 % of the patients after 1 year and 2 years respectively. This study showed encouraging clinical outcomes of DCB only treatment of de novo CTO at the 2-year follow-up, also the hard endpoints rate were low and MACE rates were acceptable.
We believe that in 2023 the aim of an interventional cardiologist should be to keep the coronaries free from metal as much as possible and to minimize the very late adverse events (15). The use of DCB in complex CAD patients appears promising and helps the interventional cardiologist in achieving this goal. Flow-limiting dissections (but not those type A and B with TIMI 3 flow) and acute recoil remain the Achille’s heelof DCB only approach. Proper preparation of the lesion with any available tool and adequate sizing of the balloon, keeping the balloon to artery ratio of 0.8-1.0 is essential for achieving the full efficacy of DCB and also will help in minimizing the acute and long term complications. Further advances in drug delivery and a better understanding of plaque morphology and careful case selection will help in treating the majority of complex CAD patients with DCB.
References
1. von Birgelen C, van der Heijden LC, Basalus MWZ, Kok MM, Sen H, Louwerenburg HW, van Houwelingen KG, Stoel MG, de Man FHAF, Linssen GCM, Tandjung K, Doggen CJM, van der Palen J, Lo¨wik MM. Five-year outcome after implantation of zotarolimus- and everolimus-eluting stents in randomized trial participants and nonenrolled eligible patients: a secondary analysis of a randomized clinical trial. JAMA Cardiol 2017;2:268–276.
2. Sharifi Z, Yazdi MJ, Eshraghi A, Vakili V, Ramezani J. Clinical outcomes and complications of treatment with supraflex stent in patients with coronary artery disease: one-year follow-up. Eur J Transl Myol 2019;29:8231.
3. Gada H, Kirtane AJ, Newman W, Sanz M, Hermiller JB, Mahaffey KW, Cutlip DE, Sudhir K, Hou L, Koo K, Stone GW. 5-Year results of a randomized comparison of Xience V everolimus-eluting and TAXUS Paclitaxel-eluting stents. Final results from the SPIRIT III trial. JACC Cardiovasc Interv 2013;6:1263–1266
4. Cortese B, D’Ascenzo F, Fetiveau R, Balian V, Blengino S, Fineschi M, Rogacka R, Lettieri C, Pavei A, D’Amico M, Poli A, Di Palma G, Latini RA, Orrego PS, Seregni R. Treatment of coronary artery disease with a new-generation drug-coated balloon: final results of the Italian Elutax SV rEgistry-DCB RISE. J Cardiovasc Med (Hagerstown) 2018; 19:247–252.
5. Latib A, Ruparelia N, Menozzi A, Castriota F, Micari A, Cremonesi A, De Felice F, Marchese A, Tespili M, Presbitero P, Sgueglia GA, Buffoli F, Tamburino C, Varbella F, Colombo A. 3-Year follow-up of the balloon elution and late loss optimization study (BELLO). JACC Cardiovasc Interv 2015; 8:1132–1134.
6. Jeger RV, Farah A, Ohlow M-A, Mangner N, Mo¨bius-Winkler S, Weilenmann D, Wo¨hrle J, Stachel G, Markovic S, Leibundgut G, Rickenbacher P, Osswald S, Cattaneo M, Gilgen N, Kaiser C, Scheller B; for the BASKET-SMALL 2 Investigators. Long-term efficacy and safety of drug-coated balloons versus drug-eluting stents for small coronary artery disease (BASKET-SMALL 2): 3-year follow-up of a randomised, non-inferiority trial. Lancet 2020; 396:1504–1510.
7.Tian J, Tang Y-D, Qiao S, Su X, Chen Y, Jin Z, Chen H, Xu B, Kong X, Pang W, Liu Y, Yu Z, Li X, Li H, Zhao Y, Wang Y, Li W, Guan C, Gao R, Xu B; for the RESTORE SVD China Investigators. Two-year follow-up of a randomized multicenter study comparing a drug-coated balloon with a drug-eluting stent in native mall coronary artery disease: the RESTORE small vessel disease China trial. Catheter Cardiovasc Interv 2020; 95:587–597.
8.Cortese B, Di Palma G, Guimaraes MG, Piraino D, Orrego PS, Buccheri D, Rivero F, Perotto A, Zambelli G, Alfonso F. Drug-coated balloon versus drug-eluting stent for small coronary vessel disease: PICCOLETO II randomized clinical trial. JACC Cardiovasc Interv 2020;13:2840–2849.
9. Louvard Y, Medina A. Definitions and classifications of bifurcation lesions and treatment. EuroIntervention. 2015;11(Suppl V):V23eV26.
10. Bruch L, Zadura M, Waliszewski M, Platonic Z, Eränen J, Scheller B, Götting B, Herberger D, Palmieri C, Sinicròpi G, Motz W. Results From the International Drug Coated Balloon Registry for the Treatment of Bifurcations. Can a Bifurcation Be Treated Without Stents? J Interv Cardiol. 2016;29:348-56.
11.Kleber FX, Rittger H, Ludwig J, Schulz A, Mathey DG, Boxberger M, Degenhardt R, Scheller B, Strasser RH. Drug eluting balloons as standalone procedure for coronary bifurcational lesions: results of the randomized multicenter PEPCAD-BIF trial. Clin Res Cardiol. 2016 Jul;105(7):613-21.
12. Köln PJ, Scheller B, Liew HB, Rissanen TT, Ahmad WA, Weser R, Hauschild T, Nuruddin AA, Clever YP, Ho HH, Kleber FX. Treatment of chronic total occlusions in native coronary arteries by drug-coated balloons without stenting - A feasibility and safety study. Int J Cardiol. 2016; 225:262-267.
13. Jun EJ, Shin ES, Teoh EV, Bhak Y, Yuan SL, Chu CM, Garg S, Liew HB. Clinical Outcomes of Drug-Coated Balloon Treatment After Successful Revascularization of de novo Chronic Total Occlusions. Front Cardiovasc Med. 2022 13;9:821380.
14. Chaddad R, El-Mokdad R, Lazar L, Cortese B. DCBs as an adjuvant tool to DES for very complex coronary lesions. Rev Cardiovasc Med 2022 14;23:13.