Anesthesia staffing refers to daily workforce planning, number of anesthetizing locations, and hours into which cases are scheduled for each such room. Calculations are done to minimize a weighted combination of the costs of too little and too few allocated hours. Managerial epidemiology studies show the value of these methods.

Hours worked exceeding allocated hours (i.e., the operating room (OR) hours into which cases are scheduled) are referred to as “hours of over-utilized OR time.” Allocated hours are calculated months before the day of surgery for each combination of service and day of the week, based upon the historical workload and the total hours of cases, including add-ons and turnovers. Surgical services are functionally defined as groups of surgeons who schedule cases into the same allocated hours (e.g., “general surgery including transplant”). Calculated OR allocations include add-on cases since they contribute to the historical OR workload. OR allocations are needed for staff scheduling, the process that determines which individual anesthesiologists, nurse anesthetists, OR nurses, and others will work each future day.
Staffing is chosen to minimize [(Cost per hour of under-utilized OR time) × (Hours of under-utilized OR time)] + [(Cost per hour of over-utilized OR time) × (Hours of overutilized OR time)]. This is one of the three simultaneous equations for the inefficiency of use of OR time, the other two being for under-utilized OR time and for over-utilized OR time, respectively. With the cost of 1 hour of over-utilized time to 1 hour of under-utilized time represented by R, (typically 1.5-2.0), the value to be minimized can be expressed in terms of hours: (Hours of under-utilized OR time) + R × (Hours of over-utilized OR time). The solution that minimizes the inefficiency in the use of OR time is insensitive to local experts’ uncertainty in the choice of the value of this parameter. The actual cost per hour is irrelevant to the mathematics, only the ratio of the cost of over-utilized to under-utilized time.
When OR allocations are calculated scientifically, based on OR efficiency, they are categorized by the combination of service and day of the week. That is because the day of the week is the best predictor of a service’s workload. Calculating an OR allocation means determining how many ORs should be staffed daily for each service and, for each of these ORs, how many hours of staffing should be planned (e.g., 8, 10, or 13 hours). Consider all possible staffing solutions for each service, individually. Start with 0 hours and progressively increase staffed hours until additional increases in the staffed hours cause the efficiency of use of OR time to decrease for that service. If shifts of 8, 10, and 13 hours are considered, then the successive choices are 0, 8, 10, 13, 16, 18 hours, etc. Increasing the staffed hours causes the efficiency of use of OR time to increase progressively to a maximum. Further increases in the staffed hours cause the efficiency to decrease, because of the progressively greater hours of under-utilized OR time. The complete enumeration can be constructed such that every series of cases performed by the same surgeon on the same day would be performed in its original sequence and take the same amount of OR time. The only change is in the start times.
For example, a surgeon is currently allocated 8 hours of OR time individually on Mondays. The surgeon historically has done 9.0 hours of cases every Monday. The hospital calculates that the expense of one hour of over-utilized time is twice that of one hour of under-utilized time, and inefficiency is expressed in terms of the number of equivalent under-utilized hours. Candidate allocations are 0, 8, 10, and 13 hours. The inefficiency of use of OR time for each potential allocation is determined by using the cost of the under-utilized and over-utilized hours that would have resulted. A 0-hour allocation would have resulted in 9 hours of over-utilized time, with an inefficiency of use of OR time proportional to 18 hours. An 8-hour allocation would have resulted in one hour of over-utilized time, with an inefficiency of 2 hours. A 10-hour allocation would have resulted in 1 under-utilized hour with an inefficiency of 1 hour. Finally, a 13-hour allocation would have resulted in 4 hours of under-utilized time with an inefficiency of 4 hours. Since the smallest value of the inefficiency of use of OR time was with 10-hours, the surgeon should have been allocated 10 hours of OR time to maximize OR efficiency. The same optimal allocation results if the hospital manager had selected a ratio of the cost of over-utilized to underutilized hours between 1.5 and 4.0.

For example, on 3 Tuesdays, a service performed 12.0, 7.0, and 15.0 hours of cases, including turnover times. There are 8-hour shifts, with overtime scheduled by rotation using a late list. The relative cost of overutilized to under-utilized hours is considered 1.75. If the service were allocated 8 hours of OR time each Tuesday, then the cost of the inefficiency of use of OR time would be proportional to 20.25 hours, where 20.25 = (0 under-utilized + 1 under-utilized + 0 underutilized + 1.75 × [4 over-utilized + 0 overutilized + 7 over-utilized]). If the allocation were two 8-hour ORs each Tuesday, the cost would be proportional to 14 hours, where 14 hours = (4 under-utilized + 9 under-utilized + 1 under-utilized). If the allocation were three 8-hour ORs each Tuesday, the cost would be 38 hours, (12 under-utilized + 17 under-utilized + 9 under utilized). Therefore, the service should be allocated two 8-hour ORs to maximize OR efficiency. Again, results are insensitive to the cost ratio of over-utilized to under-utilized hours.
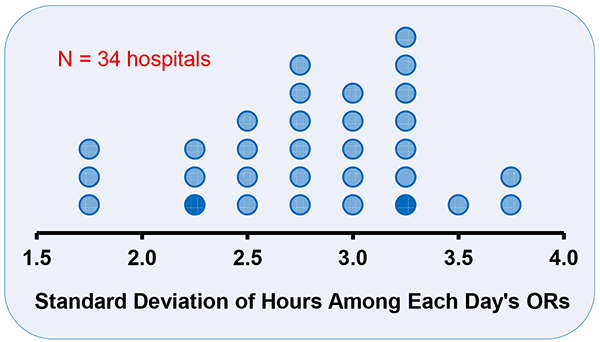
Although the analytical solution for maximizing the efficiency of use of OR time was first published more than 25 years ago, many OR managers ignore this knowledge. For managers’ efforts to reduce labor costs maximally, they need to focus on OR allocations and case scheduling because almost all anesthesia providers’ costs are labor costs. For 11 of 12 facilities studied, allocating OR time based on OR efficiency achieved significantly lower labor costs than the plans that were being used by the local managers. For 9 of 11 facilities, the statistical method approach resulted in plans that reduced labor costs by at least 10%. The percentage increases in OR efficiency were larger than 10%. The actual allocations do not match those that maximize the expected efficiency of use of OR time because, frequently, organizations plan the same allocated hours for all ORs (e.g., all services are allocated one OR for 10 hours, or two ORs for 10 hours, etc.). To appreciate why this is suboptimal, for one day, calculate the standard deviation among ORs at a facility in the workload for elective cases. Among days, for the facility, calculate the mean of the standard deviations. If suitable to use all 8-hour workdays, all 10-hour workdays, etc., then the mean of the standard deviations would be much less than one hour. However, that was not so among 34 hospitals in the United States, Australia, and France.10 All had means of at least 1.5 hours, with many greater than 3.0 hours (Figure 1). Because this variability in the durations of workdays is predictable variability, the allocated hours should be planned to match them, thereby reducing the hours that anesthesiologists, nurse anesthetists, OR nurses, etc., work late.
Suppose that anesthesiologists at a hospital report that all of the ORs finish at least an hour or two late every day. To consider the economic irrationality of the situation, suppose that the relative cost of over-utilized to under-utilized OR time were 2.0. Then, it would be twice as expensive to finish late versus early. Thus, with appropriate OR allocations, the odds for each service and OR to finish early would be approximately chances in.
Two managerial epidemiology studies show that the described matching of staffing to the workload is appropriate for “real-world” practice. Suppose that hospitals and hospital-owned ambulatory surgery centers are not limiting surgeons and patients when the cases can be performed safely sometime during a future workday selected by the surgeon. Then, during national surgical meetings, when surgeons are away, there would be fewer cases. However, during anesthesia meetings, the workload would be the same. This was observed among the 121 hospitals in Iowa, 2007 through 2016. The American Society of Anesthesiologists meeting’s Friday to Wednesday periods were compared pairwise with other such periods without holidays during the year. Caseloads were the same (+0.1%, P=0.93). In contrast, fewer general surgery cases were performed during the dates of the American College of Surgeons’ meeting (2.5%, P=0.003). Furthermore, fewer joint arthroplasties were performed during the period of the American Academy of Orthopaedic Surgeons meeting ( 5.9%, P=0.018). As another example, in the State of Florida, among patients with commercial insurance, December had more cases than November (ratio 1.108 [99% confidence interval 1.092 to 1.125]) or January (1.257 [1.229–1.286]). In contrast, among patients with Medicare insurance (traditional or managed care), December had fewer cases than November (ratio 0.917 [0.904–0.930]) or January (0.823 [0.807–0.839]) of the same year. Comparing December versus November (January) ratios for cases among patients with commercial insurance to the matching ratios for cases among patients with Medicare, years with more commercial insurance cases had more Medicare cases (Spearman rank correlation +0.36 [+0.25], both p < 0.0001). In other words, one set of cases is not negatively limiting the other set of cases.
Matching staffing to the current workload is important because most growth in surgery at hospitals occurs among surgeons who are scheduling so few cases per week that they would not be filling an OR for the day but following another surgeon in a room. All surgeons’ cases were tracked statewide over 2 years. For each surgeon, the increase in their weekly cases was calculated. For each hospital, the percentage increase in overall caseload was calculated from among the surgeons who during the first year averaged only 2 or fewer cases per week. The average hospital in Iowa had the majority of its growth in inpatient and outpatient cases from one year to the next among surgeons who performed N ≤ 2 cases per week in the baseline year (77.0% ± 2.5% [standard error]). The majority of the growth in outpatient surgery Relative Value Units was among those surgeons (81.9% ± 2.2%). Similar results were obtained for the state of Florida. The average hospital in Florida also had the majority of its growth in inpatient and outpatient cases from one year to the next among surgeons who performed N ≤ 2 cases per week in the baseline year (73.3% ± 1.5%). The majority of the growth in outpatient surgery Relative Value Units was among those surgeons (68.7% ± 0.9%).
Finally, these principles of matching staffing to workload is important because there are whole classes of proceduralists who need access to OR time to ensure that care of their patients but who will not fill an OR for the workday. Hours of daily OR time and cases were calculated among anesthesiologist pain medicine physicians at the University of Iowa and among all such physicians in the state of Florida in 2018. At least 76.6% (95% lower confidence limit) of Florida surgical facilities performing at least one neuromodulation procedure averaged fewer than 1.08 cases per two weeks. At least 89.6% of the facilities averaged fewer than 2 cases per two weeks. At least 96.5% of the proceduralists averaged fewer than 2 cases per two weeks at each facility where they operated.
References:
1. Strum DP, Vargas LG, May JH, Bashein G. Surgical suite utilization and capacity planning: a minimal cost analysis model. J Med Syst 1997;21:309 22
2 McIntosh C, Dexter F, Epstein RH. The impact of service-specific staffing, case scheduling, turnovers, and first-case starts on anesthesia group and OR productivity: tutorial using data from an Australian hospital. Anesth Analg 2006;103:1499-516
3 Pandit JJ, Dexter F. Lack of sensitivity of staffing for 8 hour sessions to standard deviation in daily actual hours of operating room time used for surgeons with long queues. Anesth Analg 2009;108:1910-5
4 Dexter F, Traub RD. How to schedule elective surgical cases into specific operating rooms to maximize the efficiency of use of operating room time. Anesth Analg 2002;94:933-42
5 Dexter F, Epstein RH, Marsh HM. A statistical analysis of weekday operating room anesthesia group staffing at nine independently managed surgical suites. Anesth Analg 2001;92:1493-8
6 Wachtel RE, Dexter F. Influence of the operating room schedule on tardiness from scheduled start times. Anesth Analg 2009;108:1889-901
7 Casimir RJ. Strategies for a blind newsboy. Omega-Int J Manage S 1999;27:129-34
8 Dexter F, Macario A. Changing allocations of operating room time from a system based on historical utilization to one where the aim is to schedule as many surgical cases as possible. Anesth Analg 2002;94:1272-9
9 Abouleish AE, Dexter F, Epstein RH, Lubarsky DA, Whitten CW, Prough DS. Labor costs incurred by anesthesiology groups because of operating rooms not being allocated and cases not being scheduled to maximize operating room efficiency. Anesth Analg 2003;96:1109-13
10 Marcon E, Dexter F. An observational study of surgeons’ sequencing of cases and its impact on postanesthesia care unit and holding area staffing requirements at hospitals. Anesthesia & Analgesia 2007;105(1):119-126
11 Dexter F, Wachtel RE, Epstein RH. Decreasing the hours that anesthesiologist and nurse anesthetists work late by making decisions to reduce the hours of over-utilized operating room time. Anesthesia & Analgesia 2016;122 3):831-842
12 Wachtel RE, Dexter F. Review of behavioral operations experimental studies of newsvendor problems for operating room management. Anesth Analg 2010;110(6):1698-710
13 Dexter F, Epstein RH. Influence of annual meetings of the American Society of Anesthesiologists and of large national surgical societies on caseloads of major therapeutic procedures. Journal of Medical Systems 2018;42(12):259
14 Dexter F, Epstein RH, Diez C, Fahy BG. More surgery in December among US patients with commercial insurance is offset by unrelated but lesser surgery among patients with Medicare insurance. International Journal of Health Planning and Management 2022;37(4):2445-2460
15 Dexter F, Jarvie C, Epstein RH. Lack of generalizability of observational studies’ findings for turnover time reduction and growth in surgery based on the State of Iowa, where from one year to the next, most growth was attributable to surgeons performing only a few cases per week. Journal of Clinical Anesthesia 2018;44:107-113
16 Epstein RH, Dexter F, Diez C, Fahy BG. Elective surgery growth at Florida hospitals accrues mostly from surgeons averaging 2 or fewer cases per week: a retrospective cohort study. Journal of Clinical Anesthesia 2022;78:110649
17 Dexter F, Epstein RH, Podgorski EM III, Pearson ACS. Appropriate operating room time allocations and half-day block time for low caseload proceduralists, including anesthesiologist pain medicine physicians in the State of Florida. Journal of Clinical Anesthesia 2020;64:109817