Precision health involves individualized approaches to patient risk screening and prevention, earlier and more accurate disease diagnosis, and personalized treatment decisions. The future of precision medicine involves population data collection and artificial intelligence approaches to integrate multi-omic information from electronic health records to improve health care quality, safety, and value.
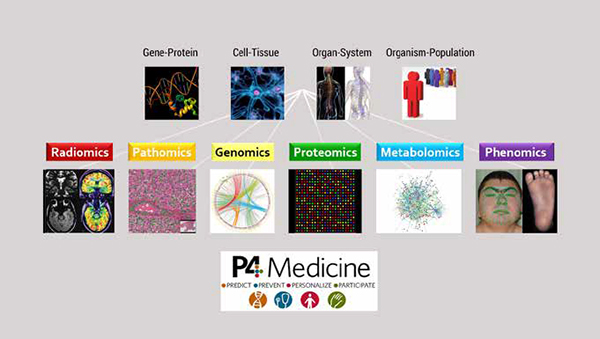
The Precision Medicine Initiative was established by the United States government in 2015 to better customize patient health care delivery based on unique genetic, environmental, and lifestyle characteristics. These goals are commonly summarized as “P4”: predictive, preventive, personalized, and participatory. In other words, precision health seeks to achieve better risk screening and disease prevention, earlier and more accurate patient diagnosis, personalized care and treatment regimens, and fully participatory decision making among patients and clinicians.
In current practice, most precision medicine efforts are based on individual genomic information: prediction of disease risk; drug, chemotherapy, and radiation susceptibility; enzyme replacement and gene therapy for single-gene disorders; and molecular therapy, immunotherapy, and cell therapy for oncologic diseases. On a larger scale, tremendous progress has been made in systems medicine, which integrates biochemical, physiologic, and environmental information on multiple scales to understand the mechanisms of health and disease. The “bottom-up” approach utilizes“omics” technologies—such as genomics, transcriptomics, proteomics, metabolomics, metagenomics, and phenomics—to collect and synthesize large volumes of molecular data. The “top-down” approach models organisms as complex mathematical systems in order to reproduce specific biological functions or phenotypes.
Theranostics is an emerging field that combines diagnostics and therapeutics. Recent updates by the World Health Organization emphasize the concept of oncologic “layered reporting” with integrated diagnostic information from genomics, pathology, and radiology. Sequential diagnosis and treatment are also becoming a reality with cutting-edge technologies such as molecular imaging and nanotherapeutics; image-guided interventions; and real-time biosensors and biofeedback.
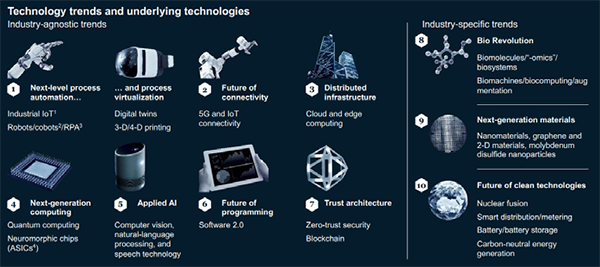
A key requirement for precision medicine is the ability to share, curate, and aggregate large quantities of data for analysis. Given the vast heterogeneity of clinical practice, there must be stringent governance standards to protect patient privacy and security, as well as systems interoperability to facilitate access, deidentification, and sharing of electronic health records. Many novel informatics platforms and digital health innovations are being driven by partnerships among academic, government, industry, and public stakeholders. These parallelsocietal technology trends including automation, virtualization, interconnectivity, and artificial intelligence (AI).
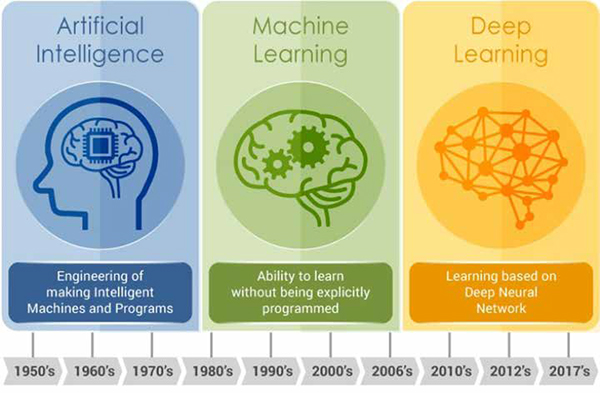
AI solutions are rapidly transforming medicine due to massive gains in computing power and infrastructure, as well as the innovation pressures of the COVID-19 pandemic. Like all disruptive technologies, AI follows a “hype cycle” with unrealistic initial hopes followed by inevitable disappointments, recalibration of expectations, and a return to steady progress. Current AI algorithms are “narrow,” meaning that they are designed to perform specific tasks such as language translation, data processing, and image recognition. Machine learning (ML) has been utilized for decades, with small amounts of structured data that require less processing power. Deep learning (DL) is a more recent development, based on neural networks mimicking the human brain in order to learn patterns from large volumes of unstructured data with minimal supervision. However, DL is data-hungry, requiring hundreds if not thousands of training cases to achieve high model performance.
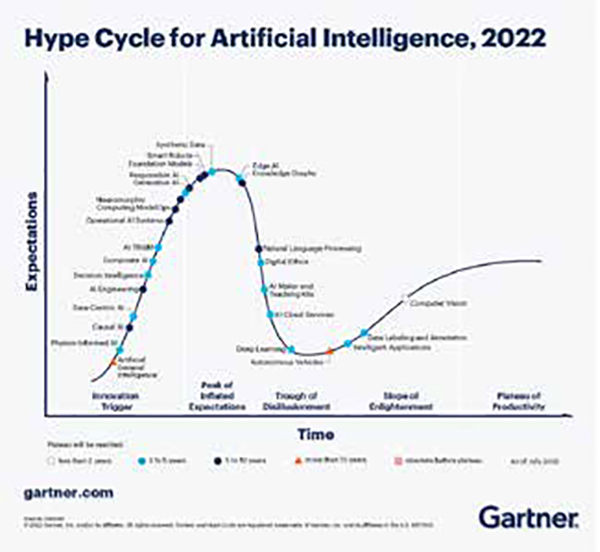
In health care, it is prohibitively expensive and impractical to acquire and maintain comprehensive datasets of patient information. Even within large organizations, data for a specific patient group or disease process can be sparse, low-quality, missing, or biased. During COVID-19, prior training data were simply not available, and situations evolved rapidly with strong geographic dependencies. As a result, institutions shifted away from big data to “small and wide”: lower-volume but diverse datasets offering greater value to local stakeholders. Recent AI advances with promise for medical applications include few-shot, transfer, federated, and attention learning. The overall challenges for health care include scalability, generalizability, and explainability. As we continue to evaluate informatics solutions, we must ensure efficient, operational, and responsible algorithms that can optimize, accelerate, and democratize healthcare delivery.
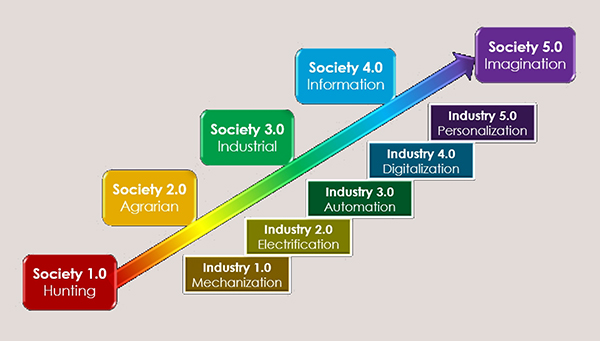
We are well into the 4th Industrial Revolution, with widespread automation, digitalization, and interconnectivity transforming our society in novel and innovative ways. Machines are beginning to perform routine daily tasks and replace traditional human work. Given the profound global workforce shortages, we have a unique opportunity to reimagine human/machine collaborations in order to maximize collective productivity, creativity, and sustainability. Such strategies are already being employed with remote patient monitoring, cobots (collaborative robots), and telemedicine appointments. At this time, AI solutions show particular promise for workflow optimization including ordering, scheduling, triage, patient notes, decision support, results communication, productivity metrics, and revenue cycle management. End-to-end automation will help free up physicians and staff time to consult with patients, interact with other departments, and maximize added value.
The Internet of Things (IoT) refers to physical objects that collect and exchange data over networks, including smart devices, mobile sensors, and wearable clothing/ accessories. These technologies enable real-time tracking of location, vital signs, physical activity, and other biometric data. Interfacing with smartphone apps or remote devices enables point-of-care evaluation and action plans, such as scheduling physician appointments, requesting medication refills, or activating emergency alert systems. The Addition of sensory (optical, haptic) feedback can provide an immersive experience (extended reality, metaverse) that facilitates social interactions such as telehealth, telerehabilitation, and teletherapy.
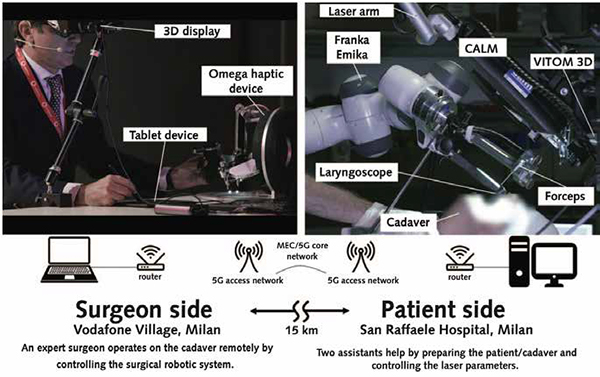
Digital health strategies are poised to democratize healthcare delivery across the globe. With the advent of population-level monitoring, socioeconomic determinants of health can be better characterized, thus informing public health interventions for disease prevention and risk minimization. Furthermore, global informatics solutions can be deployed to improve patient access with automated triage and decision support, expert consultations, and standardized medical education. Even more futuristic, the feasibility of robotic telesurgery has recently been demonstrated over wireless 5G networks, with exciting implications for remote interventions.
By leveraging advances in systems biology and information technology, we can vastly improve health care delivery by aiding consumers to make lifestyle changes; addressing underlying causes and risk factors; accelerating disease detection and diagnosis; and developing targeted treatment plans to optimize outcomes. These combined approaches will encourage the development of high-value, cost-effective systems that provide best quality care to patients across the world.