A misleading first visit is a common cause of adverse treatment outcomes. When patients can access specialists directly, their judgment in selecting a provider may be flawed. The advanced self-assessment tool, integrated with the hospital system containing doctor information, can simplify patient-doctor scheduling and improve an appropriate specialty and experience.
Misleading initial visits are a common cause of adverse treatment outcomes. When patients have direct access to specialists, their judgment in selecting a provider may be flawed. The advanced self-assessment tool, integrated with the hospital system containing doctors’ information, can simplify patient-doctor scheduling and improve the appropriateness of specialty selection and patient experience.
Scheduling an appointment with a physician is an important step in maintaining patient health and well-being and preventing diagnosis. Several factors can guide individuals in determining the optimal time to seek medical assistance.

Availability: It is an important factor when finding a physician. For instance, it is essential to consider the alignment between physicians’ office hours and patients’ schedules, which may be limited or conflict with their availability.
Timeliness: It is important to consider how quickly the patient can receive medical treatment or further diagnosis in a timely manner. The physician should promptly conduct any necessary examinations, tests, and further investigations, which can help expedite any necessary treatments or interventions.
Readiness: Patients should have some basic knowledge about their symptoms or condition, not for self-diagnosis but to facilitate discussions with the physician.
Appropriateness: Several factors need to be taken into account, including:
Clinical appropriateness: It involves selecting a physician with the appropriate specialization that aligns with the patient’s condition. Some symptoms or conditions may be related to a specific area of expertise, such as general practice, EENT, internal medicine, pediatrics, etc. Choosing a physician with the right specialization ensures that you receive the most relevant and effective care for your condition.
Financial appropriateness: It pertains to the affordability of a patient’s financial situation under their insurance plan and coverage details. It is important to consider the possibilities of exclusions for certain medical conditions under the individual patient’s insurance policy.
Service and Location: It refers to the quality of care and level of service provided by each healthcare provider, such as a patient-centric approach, accessibility, staff service mindset, atmosphere, follow-up, aftercare service, etc.
Appropriate scheduling with a physician is crucial to ensure timely and effective healthcare. However, delays in diagnosis can occur, leading to poor treatment outcomes.
Accessibility is the first step in healthcare services. Delayed or inadequate access to healthcare services often results in unfavorable treatment outcomes. Particularly in cases of cancer, delayed diagnosis and treatment are the most common consequences of poor accessibility, significantly affecting prognosis, as early-stage detection leads to better outcomes.
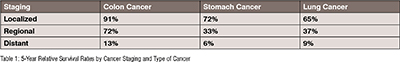
For cancer patients, referring to the American Cancer Society (ACS) treatment outcomes are mostly related to cancer staging. The 5-year relative survival rate is an indicator for measuring cancer treatment outcomes.
A relative survival rate compares people with the same type and stage of cancer to people in the overall population. For example, if the 5-year relative survival rate for a specific stage of colon or rectal cancer is 80%, it means that people who have that cancer are, on average, about 80% as likely as people who do not have that cancer to live for at least 5 years after being diagnosed. The survival rate significantly depends on cancer staging.
• Localized: There is no sign that cancer has spread outside of the organ
• Regional: Cancer has spread outside the organ to nearby structures or lymph nodes
• Distant: Cancer has spread to distant parts of the body or distant lymph nodes
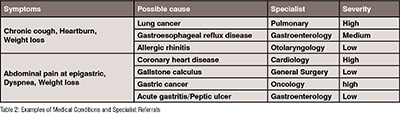
Medical knowledge limitation: Each set of symptoms can be associated with various diseases that require different medical specialties. Some symptoms cannot be predicted based solely on their lesion location. For example, abdominal pain can indicate heart disease, and coughing, typically associated with respiratory tract issues, can also be a symptom of esophageal disease. Lack of awareness among patients and even inexperienced medical staff about the intricate relationship between symptoms and diseases can lead to the oversight of serious conditions. Here is an example table showcasing symptoms, possible causes, specialists, and severity levels: (Table 2)
Illness perception – Preferences and personality types can influence how individuals react to illness, and denial reactions commonly lead to delayed diagnosis and treatment. On the other hand, an over-concerned patient is most likely to see a more critical specialist (e.g., an oncologist) with even less chance of cancer, which also leads to delayed treatment in the case of non-cancer patients.
Proper doctor arrangement– Ensuring the adequate availability of specialists is a common challenge in healthcare. Healthcare providers need to allocate sufficient resources to ensure timely and appropriate treatment for patients' conditions while aligning with the expertise of the specialists. In certain areas, doctor practices may not be directly managed by the hospital, which can further complicate doctor scheduling.
Contact point– Convenience options for patients to select doctors and make appointments facilitate timely visits. However, due to technology constraints and privacy concerns, the contact portal may not be fully open for the patient in a secure way, so direct calling for an appointment is still the main channel in some areas.
Primary care based – Although assigning a primary care physician as the first gate of evaluation, treatment, and management is the best approach for population-based healthcare management, it also has some risks especially delayed diagnosis, which may not be significant at the overall level but may be material for some individual cancer patients.
Other factors, e.g., geographic limitations.
Some of the above factors are uncontrollable from the patient and provider perspective, but there are opportunities for improvement in certain areas. For example, patient medical knowledge and perception, specialist arrangement, and appointment system can be optimized to enhance accessibility.
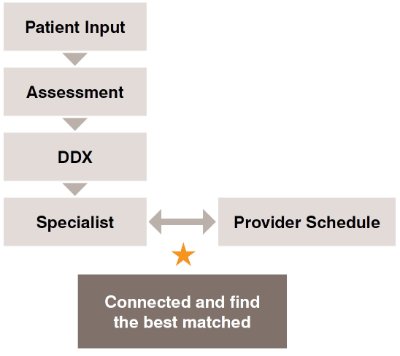
This article proposes a solution to improve accessibility in the context of healthcare systems that allow patients to directly access specialists through self-symptom assessment tools integrated with provider schedules.
In some countries, primary care systems serve as the initial point of contact for patients, with general practitioners, family physicians, or pediatricians providing a wide range of healthcare services, including health screening, diagnosis, and treatment before referring to specialists when necessary. This approach helps manage healthcare costs and reduces the workload on specialty physicians.
However, in certain situations, a “fast-track” approach to specialists may be necessary for patients with urgent concerns who require immediate consultation.
To effectively manage patient demand for healthcare services, it is essential to ensure an adequate supply of specialists appropriate for each patient's condition and to adopt responsive, just-in-time approaches to their needs.
• Patients and physicians should aim to meet as soon as possible to ensure timely access to healthcare services.
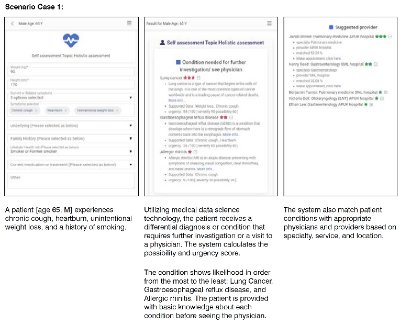
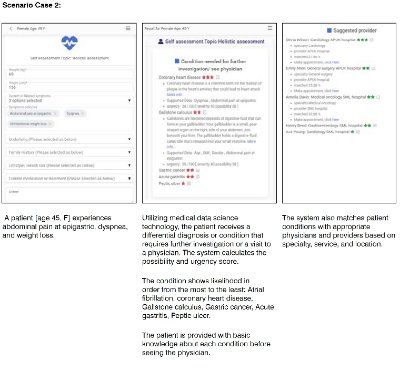
• Performing self-assessment before consulting with physicians can help patients communicate effectively. It allows them to gather valuable information about their health, such as symptoms or conditions, medical history, family history, underlying conditions, lifestyle factors, medication history, allergies, immunization history, etc. This information helps physicians understand patient health and provide appropriate care.
• Using patient input, technology, and medical data science, matching factors, can provide guidance such as:
o Patient’s likely differential diagnosis (DDX) or conditions that require further investigation or specialist consultation. The key objective is not to get the most precise diagnosis but to show a full list of possible diagnoses and their possibility scores.
o Utilizing technology, such as APIs, location tracking, or big data analysis, to match patient conditions with appropriate physicians and providers based on specialty, service, and location.
o Leveraging telemedicine and other technology-driven solutions to increase accessibility for patients, enabling them to access remote care services.
o Checking doctor availability and facilitating appointment requests, which are common features that patients need after receiving the assessment result. These features require connection technology such as API or simpler channels like email. However, ensuring a well-prepared doctor schedule in the hospital remains a key success factor, regardless of the connection channel.
Maintaining good health and well-being is fundamental to life. Delayed diagnosis and treatment can have serious consequences on a patient’s health, leading to extensive treatment requirements, poorer outcomes, and increased health risks that may lead to long-term health issues, and higher healthcare costs. The primary cause of these issues is often the mismatched and untimely visits between patients and healthcare providers.
To mitigate the risks associated with delayed diagnosis and treatment, it is crucial to use appropriate self-assessment tools that help patients choose the right provider and physician based on specialties as per their convenience. Additionally, healthcare providers must have well-organized doctor schedules to ensure good accessibility as this factor plays a major role. Lastly, integrating technology and medical data science can facilitate the connection and find the best match between a patient’s condition and an appropriate physician. This integration leads to simplified patient scheduling through self-assessment tools and hospital system integration.
--Issue 02--