Virtual Physical examination (VPExam) combines augmented reality guidance with Bluetooth stethoscopes and ECG to improve the diagnostic accuracy of assessing volume status, auscultation, and arrythmia detection resulting in 84% modification of clinical management, 40% relative risk reduction in 30-day readmissions and a 56% relative risk reduction in 30-day mortality.
Introduction
Heart failure (HF) is a leading cause of morbidity and mortality in 5.7 million Americans withmanagement costs predicted to reach 70 billion dollars by 2030. Skilled nursing facilities (SNFs) care for older patients with significant comorbidities. Morbidity and mortality rates are high for hospitalized heart failure patients discharged to SNFs with30-day readmission rates between 27 to 43%due to errors in transitions, inadequate discharge planning, and lack of appropriate follow-up with health care providers. Optimizing HF management in SNF populations is agrowing focus ofvalue-based care.
Numerous meta-analyses have demonstrated that compared to conventional care, the addition of telemedicine in heart failure management leads to reduced hospitalization and mortality.Traditional telemedicine platforms present obstacles including affordability of equipment, difficult to use technology requiring extensive training, lack of standardization, and patient privacy issues. These barriers are especially challenging to SNF and Home Care populationswith significant comorbidities, functional impairments, and barriers to transportation.
Telemedicine can offer these populations improved access, but this is typically at the expense of clinical data such as a comprehensive physical examination. Many of the most common and expensive cardio-pulmonary diseases rely on physical examination for the detection of decompensation or exacerbation. Lack of physical exam data can result in loss of early detection of clinical decompensation, reduced clinical confidence, and increased risk of misdiagnosis.
Virtual Physical Examination (VPExam) Overview
VPExam is a HIPAA compliant medical device data system that overcomesbarriers to traditional telemedicine utilizing a combination of augmented reality (AR) based guidance leading a minimally trained technician (including but not limited to nurses or medical assistants) through appropriate camera positioning for video capture based upon anatomical landmarks. VPExam augmented reality guided overlays combined with sample videos as well as text and audio instructionsteach users to obtain optimal video recordings of clinical findings such as evaluation of jugular venous distention and degree of lower extremity edema in a reproducible manner.
VPExam is integrated with Bluetooth enabled stethoscopes including the Eko Duo with single lead ECGto capture a full heart and lung exam with active user instruction. Virtual physical examination technology is customizable by provider specialty to optimize an efficient clinical workflow. The type of physical exam is customizable based on medical specialty.
Time efficient review of asynchronous clinically relevant patient management data has proven critical for ongoing physician engagement. VPExam allows nurses to transmit structured data including the manual transmission of vitals, voice recognition based virtual history and review of systems, medication reconciliation with photographs of pill bottles, and a document scanner to transmit laboratory results, orders, logs, and ECGs, etc. Providers review VPExam Physician Portal asynchronous data prior to initiating a real time HIPAA compliant video conference with the patient. The Eko stethoscope with ECG canalso be used by the provider during real time synchronous video conferencingin coordination with the nurse/ MA user with the patient. VPExam routinely transmits digital physical exam data for comprehensive assessment of volume status, cardiopulmonary auscultation, ECG detection of arrhythmias, and structured data including vitals, medication reconciliation, and labs.
VPExam also offers additional Remote Patient Monitoring (RPM) utilizing Apple Health and Google Fit Health Kit data transmission to the VPExam Provider Portal including blood glucose, body mass index, cardio fitness, blood pressure, electrocardiogram, heart rate, oxygen saturation, walking heart rate, and weight. VPExam RPM allows for transmitting alerts such as tachycardia with arrythmia from a smart watch revealing a patient going into atrial fibrillation or greater than three-pound weight gain from a Bluetooth scale revealing a patient suffering from decompensation of heart failure. Abnormal RPM data can trigger deployment of personnel to perform VPExam in patients’ home or facility for earlier physician intervention.

Takeaways from VPExam QI
Shah et al published the “VPExam Virtual Care for Heart Failure Optimizing Transitions of Care Quality Improvement Project (VPExam QI)” in the Cardiovascular Digital Health Journal, Vol 3, No 3, June 2022as a single-arm prospective comparativecommunity case studyrecruiting patients admitted for heart failure with anticipated discharge toSNFsor Home Care. Nursing satisfaction was 4.8/5 (± 0.22). 0% technical errors were detected across partners at SNFs and deployment on over 550 Home Care devices.
VPExam QI patients received clinical follow up for approximately2-3 weeks duration and data collection for 3 months following VPExam encounter. All patients approached participated and no patients elected to drop out of the study.19% of study encounters occurred with Home Care services and 81% of encounters occurred at Skilled Nursing Facilities. During the 6-month pilot, 33.8% of all hospitalized heart failure patients at University Hospitals of Cleveland Regional Hospitals were enrolled into VPExam QI with cardiology management based on guideline directed therapy.
84% of patient encounters required moderate significance changes in clinical modification based upon VPExam follow-up. The most common changes involved diuretic adjustments in 44% of encounters and vasoactive medication adjustments in 44% of encounters. Less frequent moderate significance clinical modifications included identification of medication reconciliation errors in 8% of encounters and alteration of antiarrhythmic medications in 4% of encounters. Moderate significance modification encounters were impacted by volume status assessment (47.6%), cardiopulmonary auscultation (33.3%), ECG detection of arrythmias/ atrial fibrillation (14.2%), and structured data transmission of vitals, medication reconciliation, and lab results (95.2%).
The historic control population of heart failure patients discharged from June 2020 to June 2021 had an average monthly all cause readmission rate of 15.91%. Following intervention with VPExam QI interventions,30-day hospital readmission rates dropped to 7.98%with a 40.1% relative risk reduction.In the final four of six months of VPExam QI, readmission rates fell precipitously to 0%.
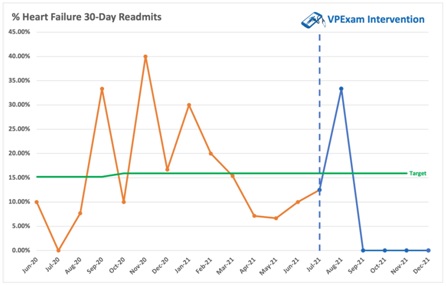
Across heart failure subtypes, patients with heart failure mortality rate following hospitalization wereapproximately 10.4% at 30 days, 22% at 1 year, and 42.3% at 5 years. 30-day mortality in VPExam QI was significantly lower at 30 days at 4.54% with a relative risk reduction of 56.3 % compared to historical controls.
Virtual Care Barriers
Significant barriers identified in the literature review preventing successful integration of quality improvement initiatives include:
1. The presentation of HF can be non-specific andmake it difficult to diagnose.
2. Guideline-directed drugs are underused due to doubt on their utility and safety concerns.
3. SNF providers are uncomfortable managing HF due to complexity and autonomy at end-of-life decisions.
4. There is mistrustand a lack of timely communication between SNF staff, patients, and their families.
5. There are limited resources in terms of diagnostic studies and access to specialists for care of patients.
6. There is poor information sharing and transfer capabilities.
VPExam QI reveals unique VPExam tools overcome many of these barriers while creating a successful local Virtual Care Network between hospital systems and Partner SNFs and Home care. VPExam deployment to SNFs and Home Care is feasible, scalable, and cost effective. VPExam Virtual Care Networks enable high compliance with follow-up with high satisfaction from nursing staff. Structured data transmission of vitals improved detection of uncontrolled hypertension as well as tachyarrhythmias often missed in traditional telemedicine. Structured data transmission of medication reconciliation often identified high risk transition of care errors. Structured data transmission of labs including renal function, brain natriuretic peptide (BNP) trends, and blood count stability improved the quality of medical decision making.
VPExam is also uniquely suited to improve clinical decisions by providing time sensitive physical exam data. Volume status including jugular venous distention and lower extremity edema influenced moderate modification management in 50% of encounters. Synchronous and asynchronous stethoscope auscultation of the heart to detect murmurs, rubs, gallops, irregularity,as well as auscultation of the lungs to detect wheezing and rhonchi influenced moderate modification management in over 31% of encounters. Synchronous and asynchronous single lead ECG transmission for arrythmia detection including atrial fibrillation influenced moderate modification management in over 13.6% of encounters.
Virtual Care Feasibility
VPExam QI results demonstrate that virtual care in transitions of care to SNFs and Home Care offer a large opportunity to improve quality of care and mitigate risk of errors for cardio-pulmonary patients. The reduction in 30-day hospitalization and mortality supports that unique Virtual Care data empowers care providers to optimize transitional quality of care.
There are also financial considerations for various stakeholders. Transfer of skilled nursing facility (SNF) residents to emergency departments are linked to increased morbidity and mortality as well as significant cost. The average cost of readmission is $15,200 across the United States.Within cardiology, there are over 233,100 readmissions for heart failure, 81,600 readmissions for cardiac arrythmias, and 74,300 readmissions following myocardial infarct annually. Other high-risk conditions with benefit from VPExam cardiopulmonary and volume status evaluation include COPD with 106,300readmissions, pneumonia with 7,500readmissions, and renal failure with 96,900 readmissions annually. VPExam helps reduce the cost of transporting patients to specialists and hospitals including ambulance cost and nursing time expenses. Virtual care also helps reduce the risk of contracting infectious diseases such as COVID while visiting the health care.In addition to the financial incentivization to utilizing virtual care to mitigate the cost of readmissions, the platform canalso increase individual provider productivity.
Virtual care offers earlier detection of clinical decompensation to underserved communities and better decisions by clinicians resulting in reduced risk of hospital admission and mortality on discharge. In turn, improved transitional care assists health care systems in preventable penalties, unnecessary care escalation, and more efficient utilization of limited inpatient and ICU beds.
Transitional Outlook of Virtual Care
Virtual care improves transitions of care for underserved SNF and Home Care patient populations. VPExam represents a promising measure to address high readmission rates in HF patients. VPExam offers capabilities to efficiently transmit virtual physical exam cardio-pulmonary and volume status assessments with supplemental structured data including vitals, medication reconciliation, and labscritical to heart failure management. Noninvasive virtual care platforms offer novel interventions to optimize the quality of care impacting readmission and mortality rates.
Future projects should focus not only on how virtual care can be integrated to provide better quality of care, but also address the paradigm of cost-effective healthcare delivery given the growing challengesof health care resource scarcity. Ongoing government and hospital support for digital innovation research allow physicians the opportunity to define the way developing technologies will be used in future workflows to optimize efficiency and quality of care.