During video-assisted or robotic-assisted minimally invasive lung surgery, the presence of pulmonary artery-adherent lymph nodes increasesthe risk ofintraoperative catastrophic events such as injury of the pulmonary artery and conversion to open thoracotomy. Preoperative workups, including bronchoscopy, help predict the pulmonary artery-adherent lymph nodes and avoid intraoperative catastrophes.
Increase in early detection of lung cancer and minimally invasive surgery
Lung cancer is the leading cause of cancer deaths in males and females. With the increase of lung cancer screening, early detection of lung cancer has been increasing. The use of minimally invasive surgery for lung cancer, including video-assisted and robotic-assisted surgery, has been increasing with growing evidence of better postoperative pain control, shorter hospitalization, lower risk of postoperative complications, and noncancer-specific mortalityassociated with these methods. During minimally invasive lung cancer surgery, unexpected injury of the pulmonary artery and conversion to open thoracotomy isunavoidable and associated with an increased risk of postoperative complications and mortality.
Pulmonary artery-adherent lymph nodes and intraoperative catastrophic events during surgery
Surgeons need to dissect lymph nodes fromthe adjacent pulmonary artery during lung cancer surgery. Those lymph nodes sometimes can firmly attach to the pulmonary artery, which causes difficulty in lymph node dissection and increases the risk of intraoperative catastrophessuch as pulmonary artery injuryandconversion to open thoracotomy (Figure 1).The research group of Shinshu University (the primary investigator, Dr. Eguchi) postulated that predicting the presence of pulmonary artery-adherent lymph nodeswould help provide patients with safer surgery, including appropriate patient selection and operative preparation. The research group conducted a retrospective cohort study of patients who underwent lung cancer surgery in Shinshu University Hospital.
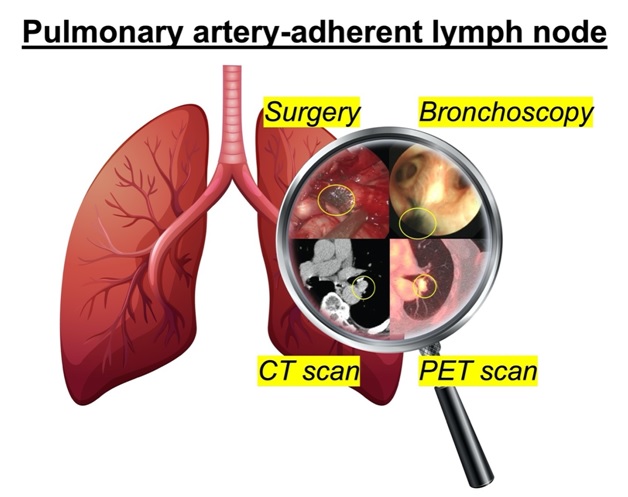
Figure 1. Schema of the pulmonary artery-adherent lymph node
Risk stratification for pulmonary artery-adherent lymph nodes
The study investigated whetherpreoperative workups including computed tomography, positron-emission tomography, and bronchoscopy can predict pulmonary artery-adherent lymph nodes. The study revealed that larger size of lymph nodes, calcification of lymph nodes, and bronchoscopic dark pigmentation were significantly associated with the pulmonary artery-adherent lymph nodes; among them, the bronchoscopic dark pigmentation was the strongest predictor. Furthermore, the presence of pulmonary artery-adherent lymph nodes was significantly associated with the injury of the pulmonary artery and the conversion to open thoracotomy during minimally invasive lung cancer resection.
The combination of lymph node size and bronchoscopic dark pigmentation successfully stratified patients’ risk of the presence of pulmonary artery-adherent lymph nodes during surgery (Figure 2). This model helps surgeons predict the risk of pulmonary artery-adherent lymph nodesin individual patients with clinically useful cutoff and good predictive performance.
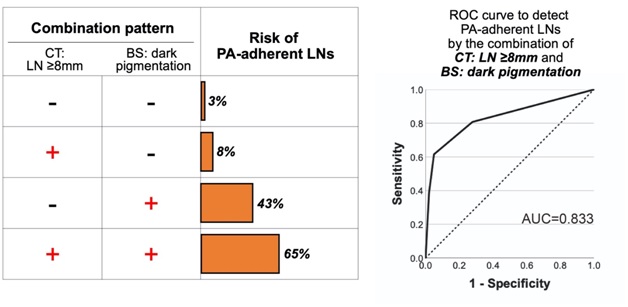
Figure 2. Risk assessment for pulmonary artery-adherent lymph nodes based on the combination of lymph node size and bronchoscopicdark pigmentation.
Lobe-specific risk of conversion and proposal of anatomical complexity of the lung
An injury of the pulmonary artery may cause a life-threatening condition or may force an extended lung removal such as a pneumonectomy (removal of the entire lungs of either side). Therefore, when surgeons encounter pulmonary artery-adherent lymph nodes during minimally invasive lung cancer surgery, intraoperative decision-making for conversion to open thoracotomy should be done to avoid further catastrophic events such as pulmonary artery injury. This may depend not only on the surgeons’ experience/skill but also on the anatomical complexity. The lobe-specific analysis in this study revealed that the impact of pulmonary artery-adherent lymph nodes on the conversion risk was higher in the right middle and the left upper lobes than the other lobes. One of the common features of these two lobes is their higher anatomical complexity than others. A schema of the anatomical complexity is illustrated in Figure 3. In cases with high anatomical complexity, a hilar dissection would become challenging with pulmonary artery-adherent lymph nodes because those lymph nodes are usually located surrounding the bronchus, resulting in multiple pulmonary-artery infiltrations, which will make safe dissection and encirclement of the lobar pulmonary artery-branch difficult byminimally invasive procedures and make surgeons elect to convert to open thoracotomy.
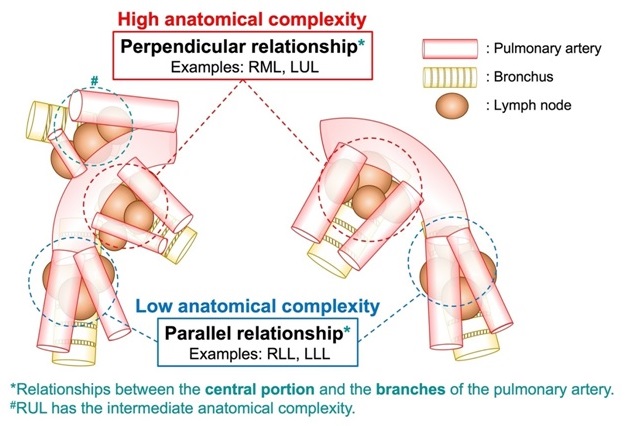
Figure 3. Schema for the anatomical complexity of the hilar structures
Patient selection protocol for minimally invasive lungsurgery
This study demonstrated its clinical utility by developing a patient selection protocol for minimally invasive lung cancer surgery (Figure 4). Notably, the protocol addressed patients without preoperative bronchoscopy as well. In high-risk patients, surgeons discuss the risk with the patients in the preoperative informed consent meeting and prepare for and prevent potential intraoperative complications by adopting measures such as avoiding assigning a trainee as the primary surgeon, preparing for blood transfusion, and administering an additional pain management such as epidural analgesia considering a potential conversion to open thoracotomy. After the initiation of this protocol in Shinshu University Hospital, patients with pulmonary artery-adherent lymph nodes were successfully detected preoperatively, and no patients underwent emergency conversions to open thoracotomy.
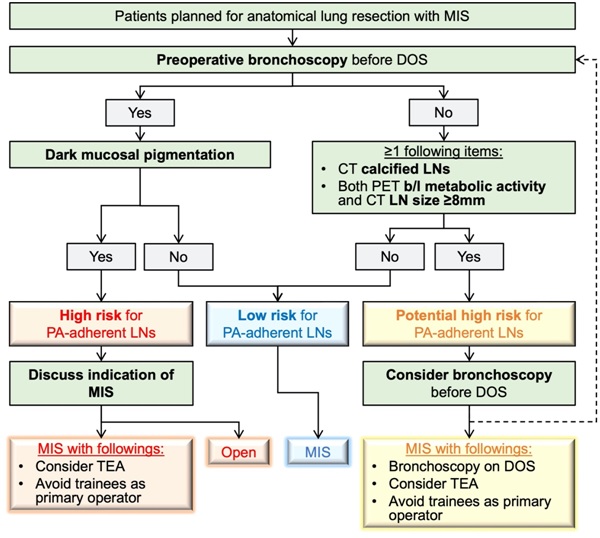
Figure 4. Patient selection protocol for minimally invasive lung cancer surgery in Shinshu University
Conclusions
In conclusion, pulmonary artery-adherent lymph nodes are associated with a high risk of intraoperative catastrophes during minimally invasive lung cancer surgery. Findings in preoperative workups such as dark bronchial pigmentation help predict tpulmonary artery-adherent lymph nodes, which can assist in enabling safer surgery.
References:
1. Bendixen M, Jørgensen OD, Kronborg C, Andersen C, Licht PB. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol 2016;17(6):836-844. (In eng). DOI: 10.1016/s1470-2045(16)00173-x.
2. Boffa DJ, Dhamija A, Kosinski AS, et al. Fewer complications result from a video-assisted approach to anatomic resection of clinical stage I lung cancer. J Thorac Cardiovasc Surg 2014;148(2):637-43. (In eng). DOI: 10.1016/j.jtcvs.2013.12.045.
3. Hristov B, Eguchi T, Bains S, et al. Minimally Invasive Lobectomy Is Associated With Lower Noncancer-specific Mortality in Elderly Patients: A Propensity Score Matched Competing Risks Analysis. Ann Surg 2019;270(6):1161-1169. (In eng). DOI: 10.1097/sla.0000000000002772.
4. Cao C, Cerfolio RJ, Louie BE, et al. Incidence, Management, and Outcomes of Intraoperative Catastrophes During Robotic Pulmonary Resection. Ann Thorac Surg 2019;108(5):1498-1504. (In eng). DOI: 10.1016/j.athoracsur.2019.05.020.
5. Puri V, Patel A, Majumder K, et al. Intraoperative conversion from video-assisted thoracoscopic surgery lobectomy to open thoracotomy: a study of causes and implications. J Thorac Cardiovasc Surg 2015;149(1):55-61, 62.e1. (In eng). DOI: 10.1016/j.jtcvs.2014.08.074.
6. Takeda T, Matsuoka S, Miura K, Hamanaka K, Shimizu K, Eguchi T. Prediction of Pulmonary Artery-Adherent Lymph Nodes for Minimally Invasive Lung Resection. Ann Thorac Surg 2022 (In eng). DOI: 10.1016/j.athoracsur.2022.01.019.
7. Byun CS, Lee S, Kim DJ, et al. Analysis of Unexpected Conversion to Thoracotomy During Thoracoscopic Lobectomy in Lung Cancer. Ann Thorac Surg 2015;100(3):968-73. (In eng). DOI: 10.1016/j.athoracsur.2015.04.032.
8. Matsuura Y, Ichinose J, Nakao M, Okumura S, Mun M. Prediction of and surgical strategy for adherent hilar lymph nodes in thoracoscopic surgery. Asian J Endosc Surg 2020;13(3):287-292. (In eng). DOI: 10.1111/ases.12763.
9. Park S, Kim HK, Park SY, Kim HK, Kim VT. Management of intraoperative bleeding in Korea. J Vis Surg 2018;4:252. DOI: 10.21037/jovs.2018.12.03.
10. Park YS, Lee J, Pang JC, et al. Clinical implication of microscopic anthracotic pigment in mediastinal staging of non-small cell lung cancer by endobronchial ultrasound-guided transbronchial needle aspiration. J Korean Med Sci 2013;28(4):550-4. (In eng). DOI: 10.3346/jkms.2013.28.4.550.
11. Yamazaki S, Koike S, Eguchi T, et al. Preemptive Intercostal Nerve Block as an Alternative to Epidural Analgesia. Ann Thorac Surg 2021 (In eng). DOI: 10.1016/j.athoracsur.2021.07.019.