It is well known that air micro pollutants can travel deep into our bloodstream through our lungs, then to our heart and systemic vessels. This would increase the risk of developing cardiovascular diseases. Air pollutants can damage blood vessels by making them narrower and harder. The scientific communities have enough data/evidence to raise awareness of this important topic.
Air pollution is contamination of the indoor or outdoor environment by any chemical, physical or biological agent that modifies the natural characteristics of the atmosphere.
The first large, prospective cohort study with more than 8 thousands participants that provided an evidence of adverse health impact of long term air pollution exposure was the Harvard Six Cities study by Dockery et al. Moreover, Lepeule, et al. conducted an extended follow up of that study from 1974 to 2009 and demonstrated that chronic exposure to air pollutants is independently related to cardiovascular mortality.
The Multi-Ethnic Study of Atherosclerosis Air Pollution Study (MESA Air), was a long term follow up study which had revealed a direct link between air pollution and atherosclerosis. The study was led by the principal investigator Dr. Joel Kaufman and found that long term exposure to micro air pollutants and nitrogen oxides at levels close to the National Ambient Air Quality Standards (NAAQS) can prematurely age blood vessels and contribute to a more rapid accumulation of calcium in the coronary arteries. This accumulation of calcium is linked to endothelial dysfunction and restriction of blood flow to the heart and other major blood vessels leading to increase cardiovascular events like heart attack and stroke.
To collect medical data, the MESA Air investigators used non-invasive exams that tracked heart health in participants over the study period. Participants received ultrasound exams to determine the thickness of the arterial wall in the arteries, CT scans to track coronary artery calcium accumulation, and blood pressure tests. Participants also received personal health recommendations based upon their test results as part of the study. Using the air quality and medical data collected, researchers determined that there was a direct link between air pollution exposure and calcium build up. The study concluded that healthy individuals exposed to air particle pollution over the long term had accelerated cases of atherosclerosis and their risk for heart attack increased. Moreover, the investigators found that the higher the exposure level, the faster atherosclerosis progresses. The study provides evidence to motivate healthcare providers to learn more about the effects of air pollution on the cardiovascular system, and the study emphasizes the importance of monitoring air quality to protect heart health.
Really, research provides evidence that short and long term exposure to particulate pollution are both linked to an increased risk of heart attacks and other forms of heart disease. The level of these pollutants has been significantly increased over the time.
Exposure to air pollutants contributed to higher blood pressure and increased incident hypertension risk. A systematic review and meta-analysis by Miao Huang, et al. has provided evidence toward a positive association between both short-term and long-term exposure to some air pollutants and blood pressure among children and adolescents.
Recently, some studies suggested that air pollution may be associated with cardiac arrhythmias. A comprehensive review performed by Dr. Shahrbaf, et al. found that Short term and long term exposure to the air pollutants can interact with the cardiac rhythms through oxidative stress, autonomic dysfunction, coagulation dysfunction, and inflammation.
The Main Air Pollutants:
The six main pollutants are carbon monoxide, lead, nitrogen oxides (NO2), ground level ozone, and particulate matter (PM), and sulfur oxides.
PM is made up of particles like tiny pieces of solids or liquids in the air. PM is considered as inhalable particles and can vary in composition and size and is usually classified into three size groups: coarse particles (PM10, diameter <10 and ≥2.5 μm), fine particles (PM2.5, diameter <2.5 μm), and ultrafine particles (<0.1 μm).
In a study conducted by C. Liu, et al., and carried out in 652 cities in 24 countries or regions across the globe, showed independent associations between short term exposures to PM10 and PM2.5 and daily all cause, cardiovascular and respiratory mortality.
In fact, PM2.5 is the pollutant with the most compelling observational and experimental evidence of association with increased risk of cardiovascular mortality.
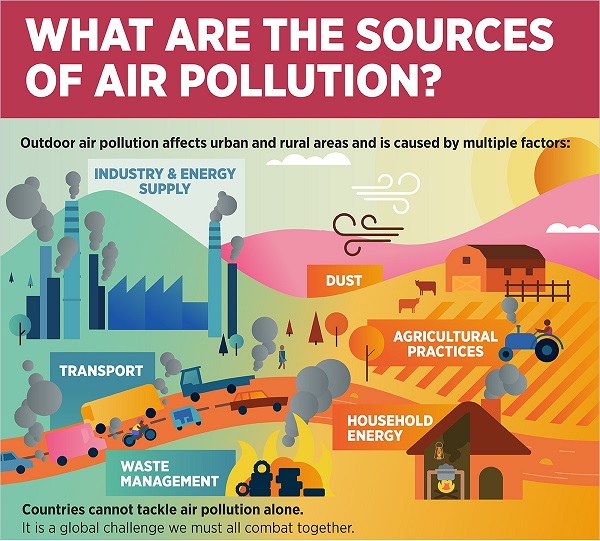
PM2.5 material is primarily formed from chemical reactions in the atmosphere and through fuel combustion. Major sources of PM2.5 include motor vehicles, smelters, power plants, industrial facilities factories, residential fireplaces and wood stoves, agricultural burning and forest fires, wind-blown dust, volcanoes, etc... Road traffic is behind a quarter of PM2.5 which is the most damaging type in urban areas.
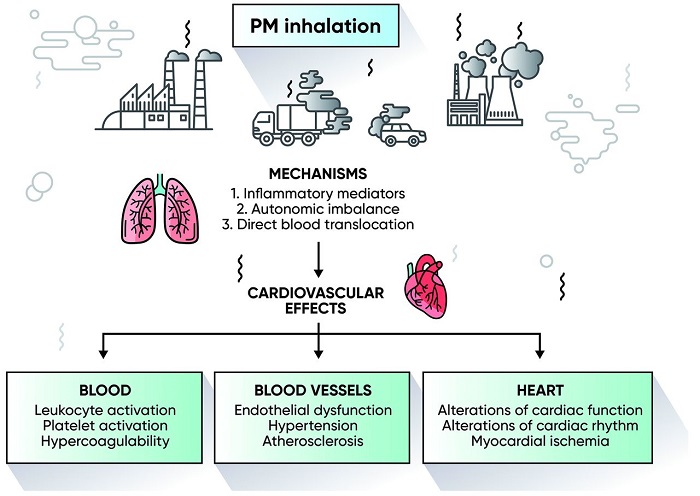
The chemical constituents of PM2.5 vary by emission source and include elemental carbon, transition metals, complex organic molecules, sulphates, nitrates, soil, and dust. PM is capable of penetrating deep into the lungs and enters the bloodstream, impacting the cardiovascular, cerebrovascular and respiratory systems.
Pathophysiology:
Several studies have been conducted to explore the pathophysiological mechanisms between air pollution and increased cardiovascular risk. The potential mechanisms are through: (1) disorders of the autonomic nervous system or sympatho/adrenal overactivity; (2) release of pro-inflammatory mediators, modified lipids or phospholipids and activation of leukocyte populations; (3) endothelial dysfunction caused by oxidative stress; and (4) activation of prothrombotic pathways.
WHO data and global awareness:
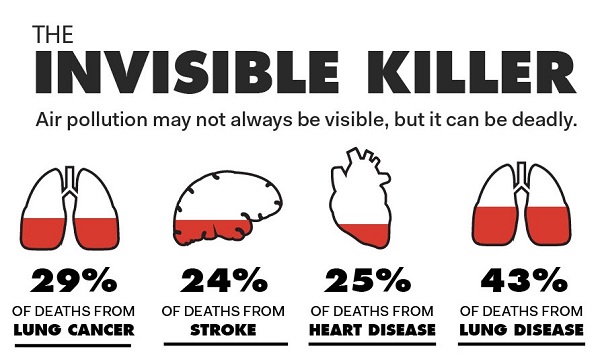
According to World Health Organization (WHO) data, almost the entire global population (99%) is exposed to air pollution levels that are higher than recommended levels. Air pollution is the known cause of over three million deaths every year due to ischaemic heart disease or stroke which is more than traditional cardiac risk factors such as diabetes, smoking or obesity. Air pollution is also the cause behind the 3% global disability adjusted life years.
In a multicentre cohort study and meta-analysis of 11 European cohorts, a 5 μg/m3 increase in annual PM2.5 exposure was associated with a 19% increased risk of incident stroke. The association was more apparent among those ≥60 years of age (HR 1.40, 95% CI: 1.05-1.87) and among never-smokers (HR 1.74, 95% CI: 1.06-2.88).
After years of intensive research and deliberations with experts across the globe, WHO updated its 2005 Global Air Quality Guidelines (AQG) in September 2021.The new air quality guidelines (WHO AQG) are ambitious and reflect the large impact that air pollution has on global health. They recommend aiming for annual mean concentrations of PM2.5 not exceeding 5 µg/m3 and NO2 not exceeding 10 µg/m3, and the peak season mean 8-hr ozone concentration not exceeding 60 µg/m3. For reference, the corresponding 2005 WHO guideline values for PM2.5 and NO2 were, respectively, 10 µg/m3 and 40 µg/m3.
Unfortunately, these WHO limits are vastly exceeded worldwide. There are data as worrying as that a non-smoker who is living in one of 30 most air polluted cities of the world would have the same cardiovascular risk as if he smoked 40 cigarettes a day.
Thanks to the overwhelming body of evidence which has accumulated over the past two decades, demonstrating that health effects of air pollution are serious and can affect nearly all organ systems of the human body. There is now broad expert consensus that air pollution is a major global public health risk factor and puts an enormous financial burden on societies. Outdoor and household air pollution together accounted for approximately 12% of all deaths in 2019. Air pollution currently ranks fourth among major risk factors for global disease and mortality, only behind hypertension, smoking and dietary factors.
The combined effects of outdoor air pollution and household air pollution are associated with 6.7 million premature deaths annually. Outdoor air pollution is estimated to have caused 4.2 million premature deaths worldwide in 2019. Some 89% of those premature deaths occurred in low- and middle-income countries, and the greatest number was in the WHO South-East Asia and Western Pacific Regions.
In terms of economic burden, the estimated global health-related external costs (i.e., those borne by society as a whole) were US$ 5 trillion in 2013 with an additional US$ 225 billion in lost labour productivity. For the WHO European Region, the overall annual economic cost of health impacts and mortality from air pollution, including estimates for morbidity costs, stood at US$ 1.575 trillion.
Air pollution is one of the greatest environmental risk to health. By reducing air pollution levels, countries can reduce the burden of disease from stroke, heart disease, lung cancer, and both chronic and acute respiratory diseases, including asthma.
Policies and investments supporting cleaner transport, energy efficient homes, power generation, industry and better municipal waste management would reduce key sources of outdoor air pollution. Access to clean household energy would also greatly reduce ambient air pollution in some regions.
Reducing the hazards:
The scientific communities (e.g., American Heart Association, etc…) provide strong arguments for supporting the public with practical personalised approaches to reducing the potential negative health effects of air pollutants. The candidates for interventions are not only people living in heavily polluted areas, but also for those at high cardiovascular risk, and those who travel to areas with high pollution.